What could microbiome analysis data reveal?
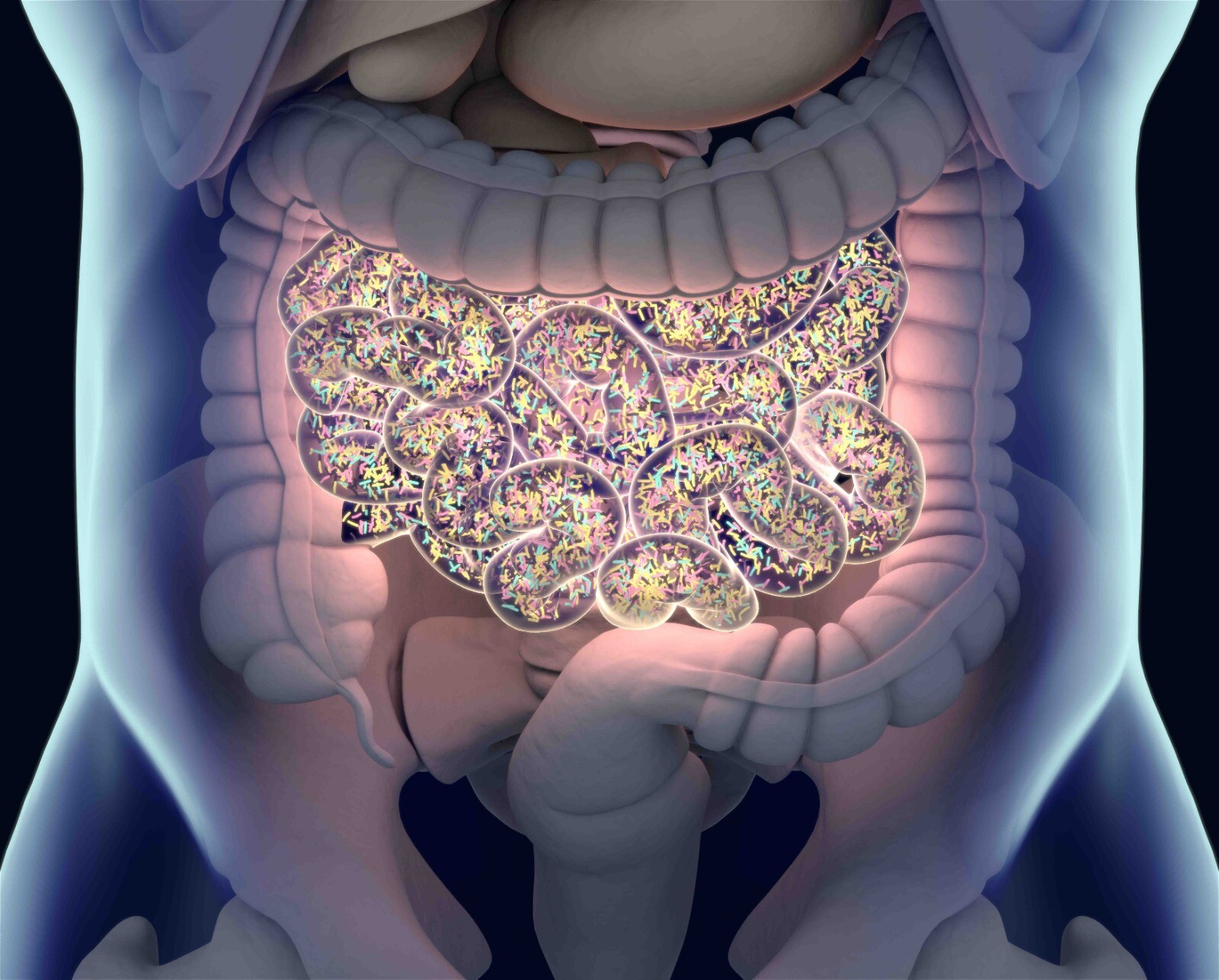
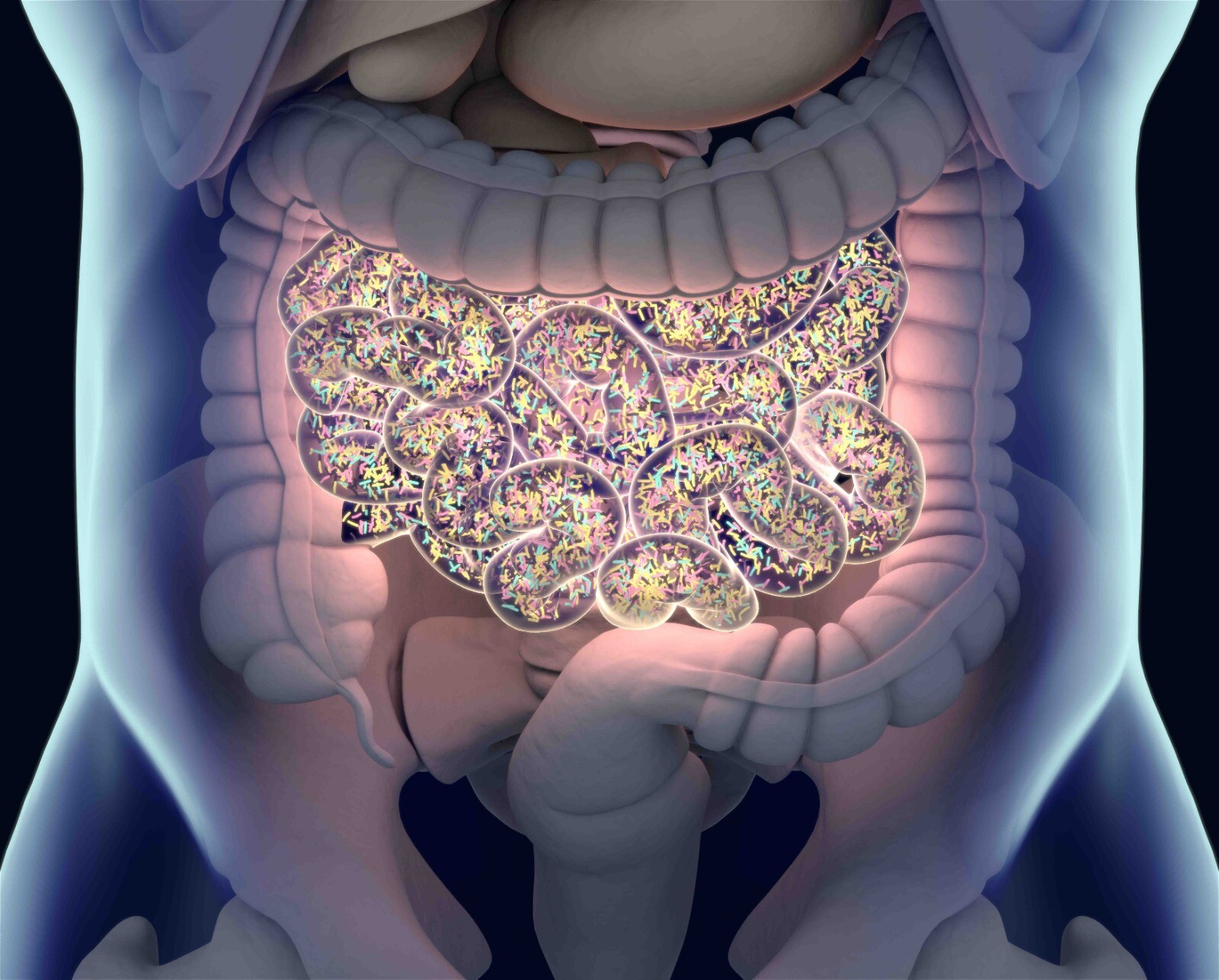
Despite the technological advances, our knowledge of the exact structure and function of the human gut microbiome remains limited. The initial activities of the HMP and other microbiome consortia focused on defining the “normal” parameters of the microbial communities in the human body. It was hoped that defining what is normal or ‘healthy’ would facilitate identification of deviations (dysbiosis) from this normal state in various diseases. A healthy gut microbiota composition is highly variable depending on age, ethnicity, lifestyle and dietary habits. However, a certain degree of gut microbiota variation, namely dysbiosis, has implications for intestinal and extra-intestinal disorders. Dysbiosis is often defined as an alteration of gut microbiota composition and a cause or a consequence of the particular disorders. Numerous studies have attempted to establish the dysbiotic state by comparing the structure and function of the microbiome between healthy and disease states. The potential dysbiotic features of the gut microbiome include the beta diversity (bacterial diversity between two groups of study population), the alpha diversity (bacteria diversity in one single individual), and the status of core essential gut microbiota or the proportion of individual signature bacteria, such as Proteobacteria phylum, Faecalibacterium prausnitzii species or Akkermansia muciniphila species.
In inflammatory bowel disease (IBD), for example, differences were seen between the microbiota of affected patients and control subjects without IBD in terms of diversity and proportions of certain signature bacteria, but it was unclear whether these differences were causative or secondary to the presence of the disease. As a result, studies have attempted to characterize the microbiota before the development of the overt disease. Those studies recruited patients at high risk for a specific disease (eg, IBD or type I diabetes) and monitored their microbiota longitudinally, comparing those who subsequently developed disease with those who did not. Other studies examined the effects of faecal transplantation therapy for specific illnesses, such as obesity and diabetes, in an attempt to establish the role of the microbiota in the pathogenesis of the disease. For diseases with well-established animal models, tests of potential causation have been attempted. A study in the UK collected stool samples from four sets of monozygotic twins with weight discrepancies, with the obese twin having a body mass index (BMI) >30 kg/m2 and a sustained BMI difference of ≥5.5 kg/m2 with their co-twin. In this twin cohort study, researchers assumed that the weight discrepancy was dependent on environmental factors alone. Faecal material from “obese” twins and “lean” twins were transplanted into two groups of mice through gastric lavage. Despite consuming the same low-fat low-calorie diet under the controlled experimental environment, mice that received faecal transplants from an “obese” twin became obese, while mice that received faecal transplants from a “lean” twin became lean. This study further illustrated the concept of a causative role for microbiota in disease manifestation.
Author: Dr Steven Loo, Professor Tsui Kwok Wing, Stephen

Recent Comments